Last week, we have discussed some details about Electronic Health Records (EHR) and some of the challenges encountered on the implementation in health care facilities. You may read it on the previous post if you haven’t.
As the concept of automation of the medical records, there has been an information system developed for the personal use of the patients. Personal Health Record, or PHR, is an electronic application—can be either web-based and/or mobile application—in which an individual can input their health information that can be easily accessed, managed; it can also be shared to others whom they authorized to view (i.e., health care providers, family members). Of course, this should be done a secure and private environment since the information within is confidential. In addition to that, PHR is separate and does not replace the legal record of any health care provider (HealthIT, 2013).
According to HealthIT.gov, there are two types of PHR:
- Standalone PHR – an independent and stand-alone application can be self-contained but can accept external data to be added on the individual’s medical record as preferred by the end-used (this can be called as well the third-party PHR).
- Tethered/Connected PHR – this is the PHR that is connected to an organization or health care facility’s EHR system or a health plan/insurance’s plan system (this can be either identified as payer-tethered or provider-tethered).
- An additional as envision in the future of PHR: Interoperable PHR – which is based on the standards for electronic healthcare data exchange (Kaelber and Pan, 2008).
There has been increase interests in signing up for PHR worldwide due to the convenience and benefits it brings to the individuals who use PHR. Some are enumerated below:
- increased patient access to credible health information and data
- improvement on the engagement and involvement of the patient in terms of personal health and disease management over time
- tracking and management of chronic diseases in collaboration with multiple HCP
- ability to detect early onset of disease and early intervention
- improved communication between patients and HCP
- lessens the incidence of repeated and unnecessary laboratory exams due to lost laboratory results
- portability of the records (especially when the individual changes location and HCPs)
- Encourages Family Health Management
- Easy verification of the details in the PHR if connected to an organization or health care facility EHR
Regardless of the evident benefits that PHR may cause, there are no specific studies that shows that it has been effective or being widely used; and there are also identified gaps and barriers that hinders the adoption of the PHR. I have cited some below:
- technical barriers: data being entered manually by the users/consumers that is quite time-consuming and prone to error, which leads to
- Health care providers being legally responsible for relying on inaccurately patient-entered health data to make decision about continuity of care of the patient
- lack of useful functionalities of the application that has no value to the patients and the HCPs; including interoperability functions.
- Lack of internet access
- Some may have cost and not all users are willing to shell out amounts of money without proof of benefit
- Due to costs of development and maintenance, lack of users, some of the projects/PHR are discontinued
- health and computer literacy of the end-users—those with low and limited literacy when it comes to health and computers are from the population of >65 years of age, low-income, immigrants, with chronic mental and physical conditions (Kahn et al, 2009).
As an individual who will utilize this kind of platform, what are the qualifications to look for? This is in line as well with this week’s driving question: What features are considered critical or most useful by users of Personal Health Records? In overview, the PHR should have the following criteria and rating per tried PHR:
- The interface should be easy to navigate and user-friendly
I think it should be taken into mind that not all users are tech-savvy and computer literate. If there may some background on how to use it, it would be beneficial if the amount of details shown in screen are limited, organized, or at least collapsible per category or area so it would not be confusing to the user. Also, it would be convenient as well if the user will not have to enter so much details because it is so time-consuming.
App MHV (3/4) – it has a collapsible side bar of the categories which is easy to view and navigate without leaving the home page. Also, it appears that side bar stays put for easy access. In the home page also shows the summaries of the inputs per category.

App WMD (3/4) – same with MHV, the sidebar is also easy accessible and stays even during page transfer to a category page. There are also legends to indicate the severity of the condition.

2. Has a great amount of security and privacy
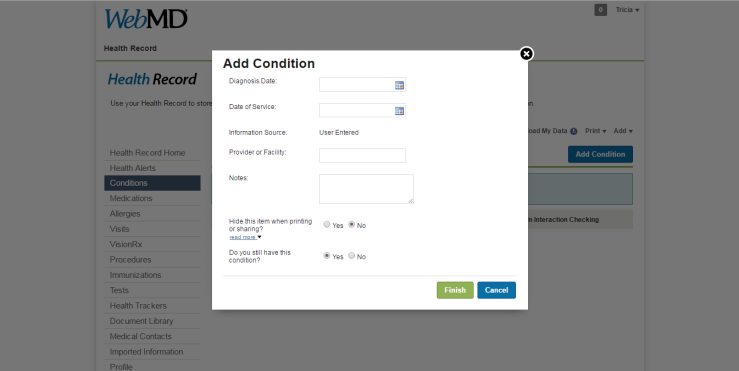
Aside from the required username and password registration/log-in for the access, there should be as well a selection of which data can be hidden when the medical report extracted from the PHR. In addition to that, unnecessary details pertaining to the personal information of the individual should be limited as well. In addition to that, it is stated in their User Agreement and Privacy Policy the importance of protecting the individual’s data and sharing of the personal data will not be disclosed unless agreed to or under any circumstances (i.e., legal procedures).
App MHV (2/4) – has the standard username and password log-in; automatically logs out during long period of inactivity. It also has an emphasized consent upon registration as seen below:

App WMD (2/4) – same with MHV; but it has an added feature to hide specific details if preferred by the user (see below for the screen capture).
3. Portability or the ability to be accessed anytime and anywhere as needed by the user, especially during emergencies
App MHV (2.5/4) – the website can be easily accessed and it also have a counterpart mobile app.
App WMD (2/4) – the website can be easily accessed but the downside is it doesn’t have a counterpart or mobile app version.
4. Have the ability to capture the diagnoses, medications, procedures done, etc
App MHV (2/4) – I initially thought that the fields are for free-text—which can lead to mismatched or incorrect spelling of the diagnoses or medicine generic names. It took a while before the drop-down suggestions appear. The end-user might not be able to know that and may have entered the items in free-text.

App WMD (2.5/4) – it has a very specific list per category for the individual to choose from. It also have the ability to add a tracker in relation to the items that are not in the list.
5. Have a way for import/export of the data
App MHV (2.5/4): It has a functionality for having specific options and range on the export of the data needed. It can also import data from the HCPs as long as the format is Continuity of Care Document (CCD) or Continuity of Care Record (CCR) format or the Blue Button format.

App WMD (1.5/4) – there is no specific range in the printing of the report and there might be a need to individually tick the hide features per category (see #2 for this app) and it is very much time consuming. Although this site has a log-in for providers and organizations/insurance where they can view the PHR of the individual (once authorized).

To summarize:

I may have missed out some features since I wasn’t able to input all the information per category but we have to take into mind that there are still missing functionalities per PHR but I think it will be more useful depending on what medical information the individual wanted to capture for their reference.
References:
- Health IT gov (2013). What are the benefits of personal health records? https://www.healthit.gov/providers-professionals/faqs/what-are-benefits-personal-health-records
- Kaelber, D., & Pan, E. C. (2008). The Value of Personal Health Record (PHR) Systems. AMIA Annual Symposium Proceedings, 2008, 343–347.
- Tang PC et al. Personal Health Records: Definitions, Benefits and Strategies for Overcoming Barriers to Adoption. J Am Med Inform Assoc 2006;13:121-126 http://jamia.bmj.com/content/13/2/121.full.pdf+html
- Kim MI and Johnson KB. Personal health records: evaluation of functionality and utility. J Am Med Inform Assoc 2002;9:171-180http://jamia.bmj.com/content/9/2/171.full.pdf+html
- How patients can improve the accuracy of their medical records. eGEMs (Generating Evidence & Methods to improve patient outcomes): Vol. 2: Iss. 3, Article 10. http://repository.academyhealth.org/egems/vol2/iss3/10/
Find me elsewhere:

[…] through a Provider’s Health Information System or for personal use by the utilization of third-party PHR applications. To reiterate the goal of e-Health—be it on the local or worldwide level—is to have quality […]
LikeLike